Dr. Peter Rentrop, an internationally renowned cardiologist, tells us that the question “I have been told that I may have coronary artery disease, what should I do?” is one we hear every day in our practice. “This is not surprising,” he continues, “since one of three women and every other man of middle age will develop coronary artery disease or CAD in their lifetime, and CAD is responsible for about one third of all deaths among middle aged or elderly Americans.”
What is CAD and how do I know if I have coronary artery disease?
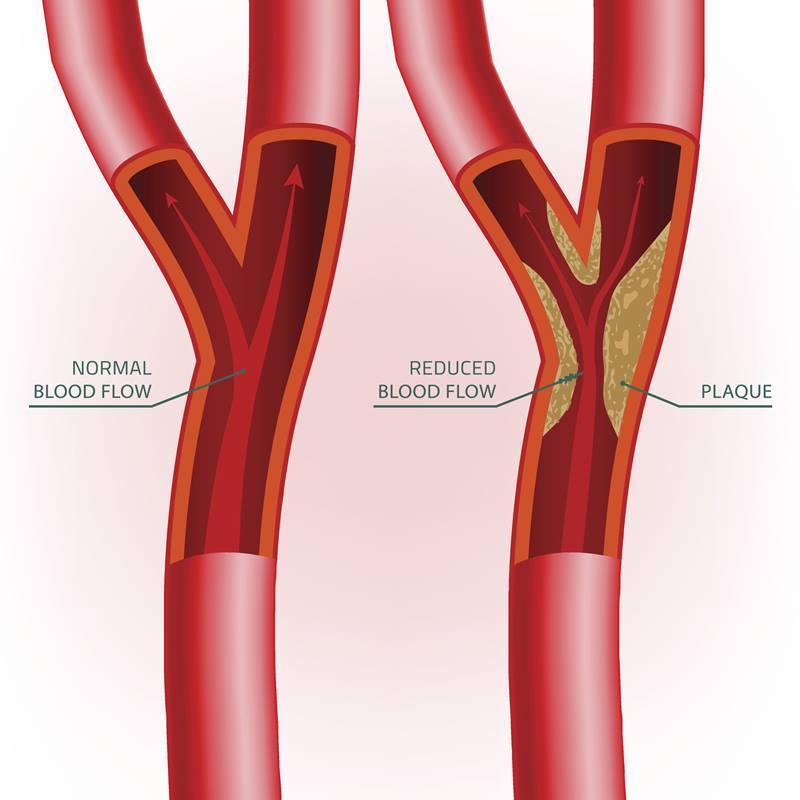
Dr. Rentrop says, “Coronary artery disease narrows the arteries of the heart, called the coronary arteries, and limits the flow of oxygen-rich blood to the heart muscle (myocardium). This narrowing, known as atherosclerotic plaque, begins in childhood with the deposition of cholesterol and other substances in the inner layers of the coronary arteries. The fatty deposits grow slowly over time, bulge into the vessel’s channel and trigger an inflammatory process within the plaque which leads to scar formation and finally calcification.
“Plaques can rupture into the artery’s channel. The rupture will be sealed rapidly by a blood clot or thrombus which forms on top of the plaque, worsening the narrowing of the artery. When a small plaque ruptures, the blood clot usually does not obstruct the coronary artery completely; rather, it organizes and retracts partially in the healing phase, but it leaves a blockage of greater severity.This process of rupture, clot formation, organization, and partial retraction tends to recur and progressively narrows the vessel. The blood flows through a narrower and narrower artery.”
“With increasing severity of the underlying blockage, plaque rupture and thrombus formation are, however, not always relatively benign occurrences. In fact, they can be catastrophic. Even a small blood clot can close a severely narrowed coronary artery completely. Cut off from its blood supply, the downstream heart muscle dies. The patient suffers a heart attack or a myocardial infarction which can be fatal.”
How does coronary artery disease affect health?
Dr. K Peter Rentrop states, “The effect of CAD on a person’s health depends on the severity and extent of the blockages and the stability of the plaque. A single, short plaque which narrows the coronary artery by less than 50%, does not limit the blood flow needed by the heart even during maximal exercise. Therefore, people are not aware of any symptoms.“
“However, coronary artery narrowing of more than 50% restricts the blood flow and oxygen supply needed by the heart during physical or emotional stress which require an increased supply. We call this obstructive CAD. The oxygen deficit of the heart muscle which results from insufficient blood flow, is called myocardial ischemia. During myocardial ischemia patients become aware of symptoms, typically chest discomfort, called angina pectoris. If the angina symptoms occur after certain activities or stressors and are promptly relieved with rest, we speak of stable coronary artery disease.”
Dr. Rentrop wants to emphasize that “the above description of CAD and its symptoms is a summary of early research. It is recognized now that many patients with obstructive CAD, particularly women and patients with diabetes, experience symptoms that are different from typical angina pectoris, such as shortness of breath. In fact, diabetic patients frequently do not notice any symptoms at all with ischemia (silent ischemia) or may not notice symptoms even when they suffer a heart attack (silent infarction). This is due to nerve damage caused by diabetes. The lack of warning signs places such patients at increased risk and may require regular testing for CAD.”
“Furthermore, we know that the effect of blockages on blood flow depends not only on their severity but also on their length. A long narrowing even if it is only 30% can limit flow as much as a short blockage of 80% and it can cause symptoms. Patients who have symptoms but have blockages that are less than 50%, have what is called non-obstructive CAD.
CAD can become unstable when a plaque ruptures and the resulting thrombus abruptly decreases blood flow to the heart. A patient may notice sudden worsening of effort tolerance or notice an increase in symptom severity. Or there may be the crushing, persistent chest pain associated with nausea and profuse sweating, indicating a heart attack which requires immediate medical attention.”
Peter Rentrop notes: “Symptoms of myocardial infarction can also be atypical and misleading.” He had a patient who had been admitted to an orthopedic unit because of excruciating left shoulder pain but was in the throes of a heart attack.
How is CAD treated?
Dr. Rentrop emphasizes, that physicians can now help most of their patients with CAD to live a normal, productive life. This usually involves risk factor modification with lifelong lifestyle adjustments and medications.
“The most important lifestyle adjustments are cessation of smoking, a heart healthy diet such as the mediterranean diet and an exercise program such as walking for half an hour on most days. Smokers are at particular risk even at a young age, when their plaques are still small.“ In a study Dr. Rentrop coauthored, every patient who sustained a heart attack under the age of 40 was a smoker. In these patients rupture of a small plaque was likely followed by formation of an unusually large blood clot triggered by smoking, which obstructed the vessel completely. Nonsmokers in the same study had heart attacks at an older age, when their plaques were more severe and even small clots could occlude an artery.
“Other risk factors which need to be identified and managed include diabetes, abnormal blood lipids such as high cholesterol, and elevated blood pressure. Effective management of all these risk factors with lifestyle adjustments including weight loss and medication, if necessary, will not only slow down or even reverse plaque progression but also decrease the likelihood of plaque rupture with its risk of myocardial infarction and death.
“Symptoms caused by stable CAD can be controlled in most patients with antianginal medications. Risk factor control will often improve symptoms further over time due to plaque regression and may even allow reduction of antianginal medication. If the medical approach fails, however, revascularization with either percutaneous coronary intervention (PCI or coronary artery bypass surgery (CABG), will control symptoms for most patients. PCI usually involves insertion of a stent into the blocked artery, whereas CABG creates a detour for the blood flow around the blockage. If a patient has severe blockages which pose a high risk of death or heart attack, revascularization may be necessary regardless of symptoms.
“Unfortunately, most patients with CAD are currently under-treated for a variety of reasons. Failure to control risk factors optimally, however, reduces the potential benefits of treatment. Dr. K. Lance Gould and associates recently showed that addition of a comprehensive program of risk factor modification to standard current medical therapy cut mortality almost in half, reduced the incidence of heart attacks and need for invasive revascularization by more than one third, and achieved substantial cost savings to the healthcare system. It is to be hoped that the results of Gould’s large, carefully conducted randomized trial will prompt insurance companies to cover scientifically tested comprehensive programs of risk factor modification.




Leave a comment